The Breast Cancer Aotearoa Coalition (BCAC) does not support the use of thermography as a breast cancer screening or diagnostic tool as we believe there is insufficient evidence of its effectiveness. We continue to recommend screening and diagnostic mammograms for the early detection and treatment of breast cancer in New Zealand.
The following detailed information on thermography was presented in the recent position statement jointly written by New Zealand’s National Screening Unit (NSU), the Cancer Society of New Zealand and the Breast Cancer Foundation New Zealand, entitled ‘The use of thermography as a breast cancer screening or diagnostic tool’.
What is thermography?
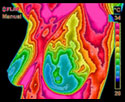
Clinical thermography is the recording of heat distribution in order to form an image (a thermogram) of the temperature distribution on the surface of the body. Thermography has been used in medicine since the 1960s and has been promoted as a tool in the early detection of breast cancer. Whilst not well understood, the underlying mechanisms for the raised temperature of a breast cancer include increased tumour metabolism and elevated blood flow. (ref. note 1)
The detection of cancer using thermography is based on differences in temperature distribution compared with the other breast. Thermography has been promoted as particularly useful in the detection of abnormalities in women aged 30–50 years, women with small breasts and women with breast implants.
History of thermography
Thermography was used and studied in the 1960s and 1970s, with up to 3,000 thermography clinics operating in the US at that time (ref. note 1). Two important trials in this period involved thermography (ref. note 1).
The first (ref. note 2) compared the use of thermography, an early form of mammography (xeromammography) and clinical examination as screening tools in a clinical trial involving 16,000 women. Thermography’s sensitivity and specificity were 39% and 82% respectively, compared with xeromammography’s 78% sensitivity and 98% specificity. In a separate trial, the Breast Cancer Detection Demonstration Project (BCDDP) planned to compare thermography, mammography and clinical examination, but dropped thermography early in the project due to a high false positive rate and low sensitivity (ref. note 3).
Following these trials, thermography was largely abandoned, bud technological advances in recent years have led to renewed interest in the technology (ref. note 1).
Thermography in New Zealand
Thermography is currently being marketed to women and general practitioners in New Zealand. The National Screening Unit, the Cancer Society of New Zealand and the Breast Cancer Foundation New Zealand have been concerned about the use of thermography as a tool in the screening and diagnosis of breast cancer, since women who undergo thermography may delay visiting their doctor with a significant symptom, or attending for screening mammography, if they believe that thermography is an adequate replacement for a doctor visit or a mammogram.
Thermography has been promoted in New Zealand as both a breast screening and diagnostic tool. Screening and diagnostic tools serve different functions and adhere to different standards.
Screening
Women are invited to participate in screening on the understanding that, overall, participating in screening will, when all the risks and benefits are considered, be beneficial to them. This is in line with international minimum standards for screening. It is vital that any new screening test is assessed through well-conducted medical research – ideally randomised controlled trials (RCTs) or meta-analyses of RCTs (ref notes 4-6).
Diagnosis
The role of a diagnostic test is to evaluate abnormalities that have been detected either clinically or by screening. To be clinically efficacious, a diagnostic test must allow a confident characterisation of the nature of a lesion and be shown to alter patient management for the better (ref note 7).
Systemic Review
In December 2003 the National Screening Unit commissioned a systematic review of the international literature on the effectiveness of thermography for population screening and diagnostic testing of breast cancer. This review was conducted by the New Zealand Technology Assessment Clearing House for Health Outcomes and Health Technology Assessment (NZHTA) – a highly respected and impartial unit of the University of Otago – using a rigorous methodology. The review was completed in July 2004.
NZHTA reviewed studies evaluating the use of infrared thermography as an adjunctive or stand-alone tool for the population screening of breast cancer and the role of infrared thermography as an adjunctive tool for the diagnosis of breast cancer.
The review established that there were no studies that evaluated the effectiveness of the infrared technology devices that are currently available in New Zealand. In addition, there were few studies that evaluated comparable infrared technologies or technologies that may become available to New Zealand. This was despite using a systematic approach, which included a comprehensive search strategy that identified 1,154 abstracts.
The review found that much of the recent literature on infrared thermography is in the form of narrative review, discussion or opinion articles. Most of the published study reports on infrared thermography refer to studies of infrared devices that are outdated or no longer available, or non-infrared methods of thermography. No studies of this technology have been conducted in New Zealand.
NZHTA concluded that the evidence that is currently available does not provide enough support for the role of infrared thermography for either population screening or adjuvant diagnostic testing of breast cancer. The NZHTA conclusions are consistent with recommendations of key professional groups. The Royal Australian and New Zealand College of Radiologists Breast Imaging Reference Group does not recommend the use of thermography for the early detection of breast cancer. (ref note 8) Similarly, the American Medical Association states that the use of thermography for diagnostic purposes cannot be recommended. (ref note 9) Thermography is not used in either the United Kingdom or Australian breast cancer screening programmes. The International Agency for Research on Cancer states that “…the sensitivity and specificity of thermography are poor, and its application to screening is unlikely.” (ref note 6).
Conclusion
BCAC agrees with and supports the conclusion reached by the National Screening Unit, the Cancer Society of New Zealand and the Breast Cancer Foundation New Zealand that there is insufficient evidence to support the use of thermography as a breast cancer screening tool or breast cancer diagnostic tool.
If any health providers are offering thermography to women, it is vital that women are fully informed of the potential harms of thermography, including the likelihood of false positive results and false negative results, and typical annual costs. This information should include an acknowledgement of the lack of proof of efficacy and effectiveness of thermography as a screening and diagnostic tool.
The Breast Cancer Foundation New Zealand has developed a detailed fact sheet that explains the differences between Mammography and Breast Thermography called Mammography and Breast Thermography in New Zealand Today.
You can view a copy of the position statement we refer to here.
References
1. Nass SJ, Henderson C, Lashof JC. Mammography and beyond: developing technologies for the early detection of breast cancer: Institute of Medicine and Commission on Life Sciences, National Research Council, 2001.
2. Feig SA, Shaber GS, Schwartz GF, Patchefsky A, Libshitz HI, Edeiken J, et al. Thermography, mammography, and clinical examination in breast cancer screening. Radiology 1977;122(1):23-127.
3. Moskowitz M. Thermography as a risk indicator of breast cancer. Results of a study and a review of the recent literature. Journal of Reproductive Medicine 1985;30(6):451-459.
4. National Health Committee. Screening to improve health in New Zealand: Criteria to assess screening programmes. Wellington: National Health Committee, 2003.
5. Muir Gray JA. Evidence-based Healthcare. 1st ed. Edinburgh: Churchill Livingstone, 1997.
6. International Agency for Research on Cancer (IARC). Breast Cancer Screening. 1st ed. Lyon, France: IARC Press, 2002.
7. Orel SG, Troupin RH. Nonmammographic imaging of the breast: Current issues and future prospects. Seminars in Roentgenology 1993;28:231-241.
8. Royal Australian and New Zealand College of Radiologists Breast Imaging Reference Group policy on the use of thermography to detect breast cancer 2001.